Motivational Interviewing – What it is and What it is not
Motivational Interviewing is a strategy that originated in the field of addiction. It was originally articulated and developed by Dr William Miller (1983) when psychology students…

Motivational Interviewing is a strategy that originated in the field of addiction. It was originally articulated and developed by Dr William Miller (1983) when psychology students…

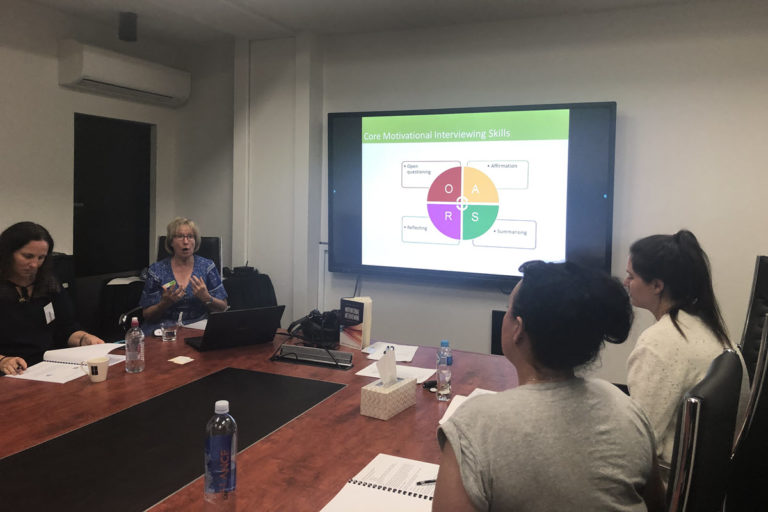
The four core motivational interviewing skills or OARS are Open questioning, Affirming, Reflecting and Summarising (Miller, W. R., & Rollnick, S. 2013). Most clinicians and helpers have these…

How often, in an attempt to ask an open ended question, have you received a closed response? Typically, asking someone “how was your day?” to hear…

The concepts of Motivational Interviewing (MI) and the Transtheoretical Model of Behaviour Change (TTM) are often linked and connected in the literature (Miller & Rollnick, 2013)….
Collaboration, compassion, evocation and acceptance underpin the spirit of Motivational Interviewing (Miller & Rollnick 2013). This spirit can best be seen in action, when the client…

At Veriti Motivational Interviewing workshops we ask participants to choose something in their own life that they are currently working on changing, or thinking of changing,…

More than 50% of GP consultations now address some form of chronic illness or disease. Lifestyle choices mean 54% of the adult population is overweight. In…

Using Motivational Interviewing (MI) enables clinicians to support and initiate behaviour change in the management and treatment of clients with chronic disease. Randomised control studies have…
Motivational Interviewing (MI) is a well-known, accepted approach to helping people struggling with behaviour change. It has been proven effective in randomised control trials across a…

Motivational Interviewing (MI) – two styles of communication with a client struggling with alcohol use Rick has been convicted of drink driving and has lost his…

Telling a person they are at risk of disease or of developing disease complications is rarely sufficient to change their behaviour. Information about risk is just…
Georgina* is a 35 year old mother of three young children. She has had asthma since childhood and frequent admissions to hospital for this, throughout her…